Article: Use Photobiomodulation ( Red Light Therapy ) To Improve Immune System Function (The Energy Blueprint) Offered in Encinitas & Carlsbad at RejuvCryo
Use Photobiomodulation To Improve Immune System Function
In numerous studies, red/NIR light therapy has proven to benefit the immune system.
In animal studies, near-infrared and red light therapy has a boosting effect on the immune system of immune-deficient cancer-inoculated animals, resulting in an increased lifespan.[216]
In human studies, photobiomodulation also boosted the immune systems and T cells of preoperative cancer patients without increasing tumor size. [217]
In the context of wound healing, it has also been shown to have beneficial effects, in part by modulating immune function.[218]
Another study found that red/NIR light therapy to the bone marrow could increase the platelet count and help resolve low blood platelets caused by chemotherapy or by an autoimmune disease.[219],[220]
It also appears to selectively modulate cell function in some types of infected cells while not affecting healthy uninfected cells in the same way.[221]
In vitro studies on human leukocytes have shown that near-infrared light can increase activity of these immune cells. Given that we know red/NIR light penetrates our blood vessels and irradiates our bloodstream, it is reasonable to think may also happen internally.[222],[223]
A fascinating study in mice looked at shining red light on the thymus gland (an important gland in the immune system) and on an area of a back leg. They found that the mice who received the treatment on the thymus gland area (in the center of the chest) had more profound changes in immune cell function.[224]
Another remarkable and more recent study from December 2017 suggests that red/NIR light may be able to slow or even reverse this “thymic involution” – thus keeping our thymus gland function and immune function in tact as we age.[225]
As discussed in the section on thyroid health, in people with Hashimoto’s – a common autoimmune condition responsible for most hypothyroidism – red/NIR light has proven to have remarkably beneficial effects on immune function.[228] Another animal model of multiple sclerosis (another autoimmune condition that degenerates the fatty sheath around nerves that helps nerve conduction) showed that just two treatments done over a span of 14 days led to significant improvement with less brain cell death and slowed the progression of the disease.[229] Other animal studies have found similar effects.[230]
Overall, red/NIR light seems to be an “immune nutrient” that supports optimal immune function in a wide variety of different scenarios and health conditions. It seems to be able to positively affect immune function in the right direction, potentially, regardless of whether someone has low immune function during an infection or has an overly active and imbalanced immune system due to autoimmune disease.
Can You Overdose on Photobiomodulation? (The Biphasic Dose Response)
As I mentioned, there is something called the biphasic dose response. But what does that mean?
That means that too little red/NIR light therapy won’t provide much, if any, benefit, and too much will also negate the benefit.
In other words, it’s important to get the dose right and to be in the range I’m recommending. You aren’t doing yourself any favors by dosing higher than my guidelines suggest.
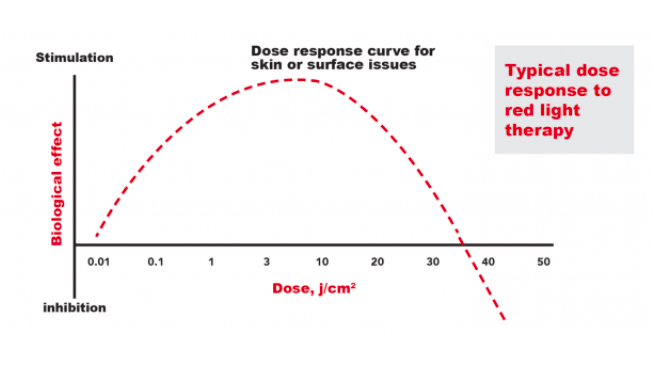
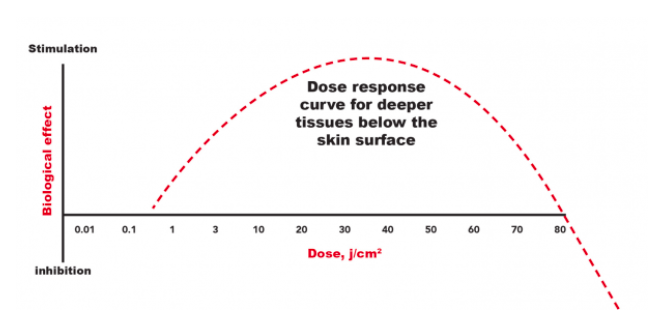
Below are two illustrations meant to give you an idea of the optimal dosing surface tissues and deep tissues. (Note: These images are not exact, because actual responses differ somewhat depending on the exact tissues treated and the type of device and other parameters used – these images are intended to illustrate the general concept of the biphasic dose response and give an idea of the general range of optimal doses.)
Here is an illustration of the general optimal dose range for skin treatments (or tissues near to the surface of the body):
Here is an illustration of the general optimal dose range for deeper tissues beneath the skin:
I know there is a tendency in human psychology to want to do more and think that higher amounts of something will be better – i.e. “if a little is good, a lot must be better.” So let me repeat one more time for emphasis: With red/NIR light treatment, more DOES NOT equal better.
Stick with the recommended dose range, start with the lowest end of the range, and don’t be in a rush to do a lot more. The benefits may be most optimal in the lower to mid-range of the recommended dosage.
References
[1] Freitas de Freitas et al. (2016) Proposed Mechanisms of Photobiomodulation or Low Level Light Therapy
[2] Hamblin, M, et al. (2018). Low-level light therapy: Photobiomodulation. Society of Photo-Optical Instrumentation Engineers (SPIE).
[3] Câmara AB, et al. (2018). Sunlight Incidence, Vitamin D Deficiency, and Alzheimer’s Disease. J Med Food. 2018 Mar 22. doi: 10.1089/jmf.2017.0130.
[4] Sorenson, M, (2016). New Research Sheds More Light on Parkinson’s Disease Sunlight Institute
[5] Wang, J, et al. (2016). Vitamin D and Sunlight Exposure in Newly-Diagnosed Parkinson’s Disease Nutrients. 2016 Mar; 8(3): 142.
[6] Tremlett, H, et al. (2018) Sun exposure over the life course and associations with multiple sclerosis American Academy of Neurology
[7] Egan, K. M, et al. (2005). Sunlight and Reduced Risk of Cancer: Is The Real Story Vitamin D? JNCI: Journal of the National Cancer Institute, Volume 97, Issue 3, 2 February 2005, Pages 161–163
[8] Holick MF, (2013). Vitamin D, sunlight, and cancer connection. Anticancer Agents Med Chem. 2013 Jan;13(1):70-82.
[9] Holick, MF, (2014) Cancer, sunlight, and Vitamin D. Journal of Clinical & Translational Endocrinology Volume 1, Issue 4, December 2014, Pages 179-186
[10] van der Rhee, H.J, et al. (2006). Does sunlight prevent cancer? A systematic review EJC September 2006 Volume 42, Issue 14, Pages 2222–2232
[11] Fleury, N, et al. (2016). Sun Exposure and Its Effects on Human Health: Mechanisms through Which Sun Exposure Could Reduce the Risk of Developing Obesity and Cardiometabolic Dysfunction Int J Environ Res Public Health. 2016 Oct; 13(10): 999.
[12] Gorman, S, et al. (2017). Ultraviolet radiation, vitamin D and the development of obesity, metabolic syndrome and type-2 diabetes. Photochem Photobiol Sci. 2017 Mar 16;16(3):362-373. doi: 10.1039/c6pp00274a.
[13] Fleury, N, et al. (2016). Sun Exposure and Its Effects on Human Health: Mechanisms through Which Sun Exposure Could Reduce the Risk of Developing Obesity and Cardiometabolic Dysfunction Int J Environ Res Public Health. 2016 Oct; 13(10): 999.
[14] Gorman, S, et al. (2017). Ultraviolet radiation, vitamin D and the development of obesity, metabolic syndrome and type-2 diabetes. Photochem Photobiol Sci. 2017 Mar 16;16(3):362-373. doi: 10.1039/c6pp00274a.
[15] Fleury, N, et al. (2016). Sun Exposure and Its Effects on Human Health: Mechanisms through Which Sun Exposure Could Reduce the Risk of Developing Obesity and Cardiometabolic Dysfunction Int J Environ Res Public Health. 2016 Oct; 13(10): 999.
[16] Frellick, M, (2016) Avoiding Sun as Dangerous as Smoking, Medscape
[17] Lindqvist, PG, et al. (2014). Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014 Jul;276(1):77-86. doi: 10.1111/joim.12251. Epub 2014 Apr 23
[18] Keshet-Sitton, A, et al. (2017). Illuminating a Risk for Breast Cancer: A Preliminary Ecological Study on the Association Between Streetlight and Breast Cancer Integr Cancer Ther. 2017 Dec; 16(4): 451–463.
[19] Al-Naggar, RA, et al. (2016). Artificial Light At Night and Cancer: Global Study Asian Pac J Cancer Prev. 2016; 17(10): 4661–4664. doi: 10.22034/APJCP.2016.17.10.4661
[20] De Nike, L, et al. (2012). Study links exposure to light at night to depression, learning issues
[21] Rybnikova, NA, et al. (2016). Does artificial light-at-night exposure contribute to the worldwide obesity pandemic? International Journal of Obesity volume 40, pages 815–823 (2016) doi:10.1038/ijo.2015.255
[22] McFadden, E, et al. (2014). The Relationship Between Obesity and Exposure to Light at Night: Cross-Sectional Analyses of Over 100,000 Women in the Breakthrough Generations Study American Journal of Epidemiology, Volume 180, Issue 3, 1 August 2014, Pages 245–250,
[23] Fonken, LK, et al. (2014) The Effects of Light at Night on Circadian Clocks and Metabolism Endocrine Reviews, Volume 35, Issue 4, 1 August 2014, Pages 648–670
[24] Science Daily, (2017). Artificial light from digital devices lessens sleep quality Endocrine Reviews, Volume 35, Issue 4, 1 August 2014, Pages 648–670
[25] De Nike, L, et al. (2012). Study links exposure to light at night to depression, learning issues
[26] Huang, Y-Y, et al. (2009) Biphasic Dose Response in Low Level Light Therapy Dose Response. 2009; 7(4): 358–383.
[27] Hamblin, M. (2008). The role of nitric oxide in low level light therapy. Proceedings of SPIE – The International Society for Optical Engineering 6846 · February 2008 with 2,541 Reads DOI: 10.1117/12.764918
[28] Hamblin, M, et al. (2018). Low-level light therapy: Photobiomodulation. Society of Photo-Optical Instrumentation Engineers (SPIE).
[29] Hamblin, M. (2008). The role of nitric oxide in low level light therapy. Proceedings of SPIE – The International Society for Optical Engineering 6846 · February 2008 with 2,541 Reads DOI: 10.1117/12.764918
[30]Farivar, S. et al. (2014). Biological Effects of Low Level Laser Therapy. Journal of Lasers in Medical Science.
[31] Sommer A.P. et al. (2015) Light Effect on Water Viscosity: Implication for ATP Biosynthesis
[32] Sommer A.P. et al. (2015) Light Effect on Water Viscosity: Implication for ATP Biosynthesis